The New Era of Women’s Health: What the FDA’s Shift on HRT Means for Your Pelvic Health
For decades, many women were told to "power through" the symptoms of menopause and perimenopause. A cloud of fear surrounded Hormone Replacement Therapy (HRT), leaving millions to navigate hot flashes, brain fog, and pelvic discomfort without support.
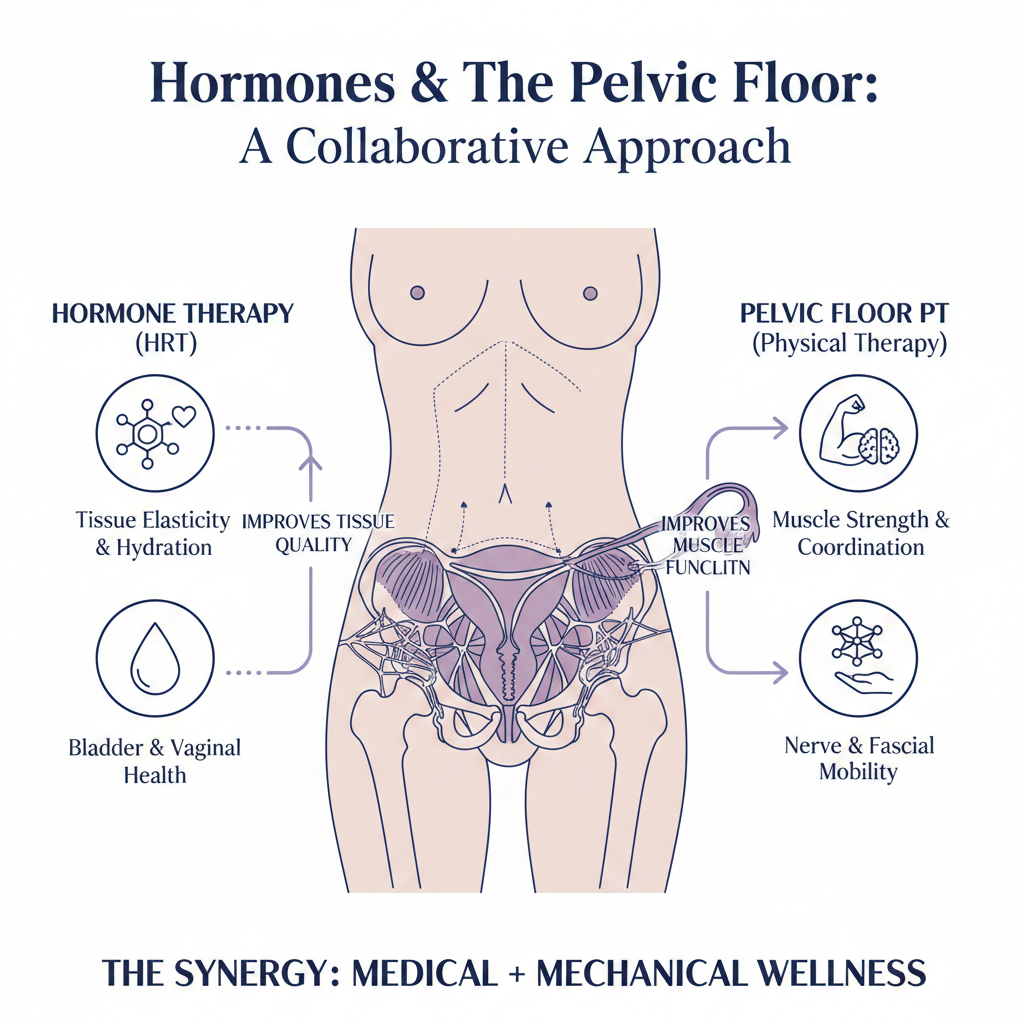
But the tide is finally turning. High-profile coverage in The New York Times and recent FDA updates have brought a new level of nuance to the conversation. We are moving away from the "one-size-fits-all" fear of the past and into an era of personalized, proactive care. For many women in NYC, South Florida, and all over the country, this means better access to the hormones that keep tissues healthy. However, as we enter this new era, it is vital to understand that while HRT addresses the chemistry of your body, Pelvic Floor Physical Therapy addresses the mechanics.
If you are navigating this transition, it is essential to understand that hormones and your pelvic floor are deeply connected.
The Hormonal Connection: Why the Pelvic Floor Changes
The pelvic floor is one of the most hormone-sensitive areas of the body. Both the muscles and the delicate tissues of the pelvic bowl are rich in estrogen receptors. When estrogen levels fluctuate or decline during perimenopause and menopause, the impact is physical:
Tissue Health: Estrogen helps maintain the thickness and elasticity of the vaginal and urethral linings. Without it, tissues can become thin, dry, and easily irritated—a condition often called Genitourinary Syndrome of Menopause (GSM).
Muscle Integrity: Hormonal shifts can affect muscle tone and the ability of the pelvic floor to support the bladder, uterus, and rectum.
The "Urgency" Spike: Declining estrogen can irritate the bladder lining, leading to increased frequency and that "I have to go right now" feeling.
Why HRT is Only Half the Story
The recent FDA moves and increased access to HRT are incredible wins for women’s health. However, medication is often just one piece of the puzzle.
Think of it this way: HRT can improve the "quality of the soil" (your tissues), but Physical Therapy "retrains the garden" (your muscles and coordination).
Benefits of HRT and Pelvic floor physical therapy done in conjunction. The Soil & Garden approach.
Even if you start HRT, your body may have spent years "compensating" for discomfort or weakness. You might have developed habits like:
Bracing or clenching to manage pelvic pressure.
Shallowing your breathing, which puts more pressure on the bladder.
Avoiding certain movements due to fear of leakage.
Hormones can restore the tissue, but they cannot un-learn those compensatory patterns. This is why the most effective approach—often cited by leading menopause specialists—is a combination of hormonal support and specialized pelvic floor therapy.
Estrogen is the lifeblood of the pelvic floor. It keeps the tissues of the vagina and urethra thick, elastic, and hydrated. When estrogen levels drop during perimenopause and menopause, we often see a spike in issues like urinary incontinence, pelvic pain, and vaginismus.
1. Resolving Urinary Incontinence
HRT helps improve the "seal" of the urethra by thickening the lining. However, if your pelvic floor muscles are weak or poorly coordinated, you may still experience leakage when you cough, sneeze, or exercise. Physical therapy trains these muscles to respond reflexively, providing the structural support that hormones alone cannot.
2. Addressing Pain and Vaginismus
For women dealing with vaginismus (involuntary tightening) or general pelvic pain, HRT is a godsend for reducing vaginal dryness and irritation. But the "memory" of pain often remains in the muscles. Specialized physical therapy uses manual techniques to desensitize the area and teach the muscles how to relax, making intimacy comfortable again.
A Collaborative Model: Your PT and Doctor in Sync
The most effective wellness plan is never a solo effort. One of the most important roles of a specialized Pelvic Floor Physical Therapist is acting as a bridge between you and your medical team.
Our overarching goal is your total wellness. This means we don't work in a vacuum. We stay in active consultation with your OBGYN, Urologist, or Menopause Specialist to ensure your medical and physical therapy management go hand-in-hand.
How this collaboration benefits you:
Calibration: We can track how your muscles are responding to different HRT dosages and provide feedback to your doctor.
Integrated Care: If a specific hormonal cream is being used to treat tissue thinning, we coordinate our manual therapy to ensure we are supporting that healing process without causing irritation.
Holistic Wellness: By looking at your health from both a medical and mechanical perspective, we ensure no "gaps" are left in your recovery.
Conclusion: A United Front for Your Health
By combining modern medical breakthroughs like HRT with specialized pelvic floor therapy, you aren't just "getting through" menopause—you are setting the foundation for a strong, active, and confident second half of life. The recent FDA moves are a landmark victory for women, but hormones are just one piece of the puzzle. By combining the chemical support of HRT with the mechanical retraining of Pelvic Floor Physical Therapy, you are giving your body the best possible chance to thrive.
When your medical and physical therapy teams are in sync, the result isn't just the absence of symptoms—it's the restoration of confidence, comfort, and vitality.